Midazolam-Induced Amnesia
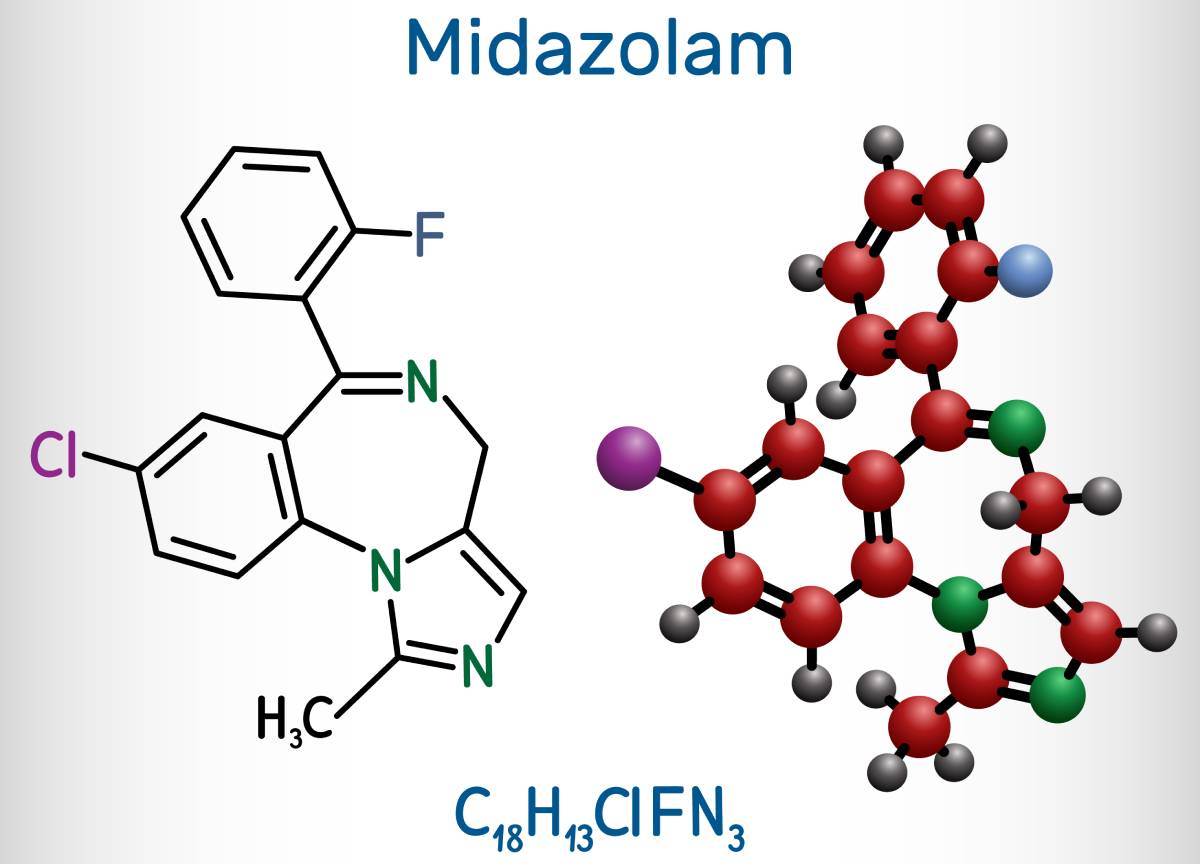
Midazolam is a potent benzodiazepine used for anesthetic purposes. It amplifies synaptic inhibition via different ʏ-aminobutyric acid (GABAA) receptor subtypes. Researchers believe this mechanism, which blocks long-term potentiation, is the reason behind midazolam-induced amnesia [1]. Specifically, neurons in the CA1 region of the hippocampal formation, which is critical for memory, are the most affected by the drug. Amnesia is a beneficial component of anesthesia as many procedures and surgeries are traumatic, and remembering the event (e.g. if the patient is not unconscious under general anesthesia) can be harmful. Previous studies have also suggested that midazolam decreased preoperative anxiety in children, which is associated with poorer outcomes, and decreased the incidence of postoperative psychological concerns, such as nightmares, eating disturbances, or enuresis, possibly due to the amnesic effect of the drug [2].
The molecular targets of midazolam in the CNS are GABAA receptors, pentametric ligand-gated chloride channels that, when activated, hyperpolarize neurons, and cause their inhibition [3]. A recent 2022 study assessed the molecular aspect of midazolam-induced amnesia through acutely prepared brain slices of mice. At a concentration of 10 nM, comparing the long-term potentiation-suppressing effect of midazolam in α1-, α5-, α1/2/3-, α1/3/5– and α2/3/5-GABAA subtypes knock-in mice strains pointed to a dominant role for the α1– GABAA subunit in producing amnesia. On the other hand, they found no change in α2/3/5-GABAA receptor activation at this low nanomolar concentration. However, at higher concentrations (500 nM), midazolam enhances the charge transfer of miniature synaptic events, activating α1– GABAA receptors as well as α2/3/5-GABAA receptors [1]. These conclusions indicate that midazolam has different concentration-dependent binding affinities for α1– and α2/3/5– subunits.
Preterm infants are subjected to many stressful and potentially painful procedures during neonatal care; therefore, sedation therapies are essential, opioids and benzodiazepines among the most commonly employed strategies [4]. In a study of 138 neonates undergoing magnetic resonance imaging and diffusion tensor imaging (DTI), total midazolam dose predicted decreased hippocampal volume but an increased mean diffusivity rate (MD; this measure is typically consistent with increased water content, for example in the cases of edema or inflammation). Increased MD causes abnormal hippocampal growths, which were associated with lower cognitive score, midazolam dose, and surgery [5]. Following their findings, the researchers advise against use of midazolam in preterm infants, particularly those who do not require surgery or invasive procedures.
Several studies have indicated midazolam induces anterograde, but not retrograde, amnesia [7]. A clinical study of 40 surgical patients undergoing anesthesia tested visual recognition and recall for events before and after the administration of different doses of midazolam [2]. There was no evidence of retrograde amnesia in any of the participants, and after midazolam administration, patients receiving the drug remembered fewer items and events than the control patients in a dose-dependent manner, indicating the presence of anterograde amnesia. Interestingly, there was a significant difference of recall rate for patients receiving higher doses of midazolam, resulting in lower recall in the event in question – in this case, mask oxygenation. According to the study procedures, the measurement was timed to occur simultaneously with midazolam administration; taken together, this finding suggests the possibility of near-instantaneous anterograde amnesia (memories of events up to this point were not affected). The authors suggest that midazolam administration during anesthesia may be influenced by the effects of co-administered drugs, and the resulting amnesia is a byproduct of this drug-drug interaction [2].
Anterograde midazolam-induced amnesia may be beneficial for young children and other patients, as it would decrease their anxiety before surgery. Some studies have also implicated the drug’s more harmful components – particularly abnormal hippocampal growth. The nuances of midazolam and guidelines on its administration should be established through further thorough investigations.
References
- Puig-Bosch, X., Bieletzki, S., Zeilhofer, H. U., Rudolph, U., Antkowiak, B., & Rammes, G. (2022). Midazolam at Low Nanomolar Concentrations Affects Long-term Potentiation and Synaptic Transmission Predominantly via the α1–γ-aminobutyric Acid Type A Receptor Subunit in Mice. Anesthesiology, 136(6), 954–969. https://doi.org/10.1097/ALN.0000000000004202
- Kain, Z. N., Hofstadter, M. B., Mayes, L. C., Krivutza, D. M., Alexander, G., Wang, S.-M., & Reznick, J. S. (2000). Midazolam: Effects on Amnesia and Anxiety in Children. Anesthesiology, 93(3), 676–684. https://doi.org/10.1097/00000542-200009000-00016
- Forman, S. A. (2022). Γ-aminobutyric Acid Type A Receptor Subtypes and Circuit Connections in Midazolam-induced Amnesia, Sedation, and Hypnosis. Anesthesiology, 136(6), 880–882. https://doi.org/10.1097/ALN.0000000000004234
- Rajendram, R., Patel, V. B., & Preedy, V. R. (2022). Long-term Effects of Anesthesia on the Brain: An Update on Neurotoxicity. In Treatments, Mechanisms, and Adverse Reactions of Anesthetics and Analgesics (pp. 195–209). Elsevier. https://doi.org/10.1016/B978-0-12-820237-1.00019-3
- Duerden, E. G., Guo, T., Dodbiba, L., Chakravarty, M. M., Chau, V., Poskitt, K. J., Synnes, A., Grunau, R. E., Miller, S. P.
Midazolam dose correlates with abnormal hippocampal growth and neurodevelopmental outcome in preterm infants. (2016). In Annals of Neurology, 79(4), 548-559. https://10.1002/ana.24601
- Veselis, R. A., Reinsel, R. A., Feshchenko, V. A., & Wronski, M. (1997). The Comparative Amnestic Effects of Midazolam, Propofol, Thiopental, and Fentanyl at Equi-sedative Concentrations. Anesthesiology, 87(4), 749–764. https://doi.org/10.1097/00000542-199710000-00007
- Dundee, J. W., & Wilson, D. B. (1980). Amnesic Action of Midazolam. Anesthesia, 35(5), 459–461. https://doi.org/10.1111/j.1365-2044.1980.tb03822
