Long-Term Immune Response after COVID-19
After two years studying the symptoms and pathology of the infectious disease caused by the SARS-CoV-2 virus, researchers have begun to explore the long-term physiological consequences and immune response following COVID-19 infection. Although much of this research remains in the early stages, the results point to some enduring protection for individuals across the globe who have suffered infection or received vaccinations. So far, research suggests that the primary long-term immune responses retained by patients following COVID-19 infection include T and B cell memory, allowing long-term production of SARS-CoV-2-specific antibodies and neutralization of the virus to a degree.
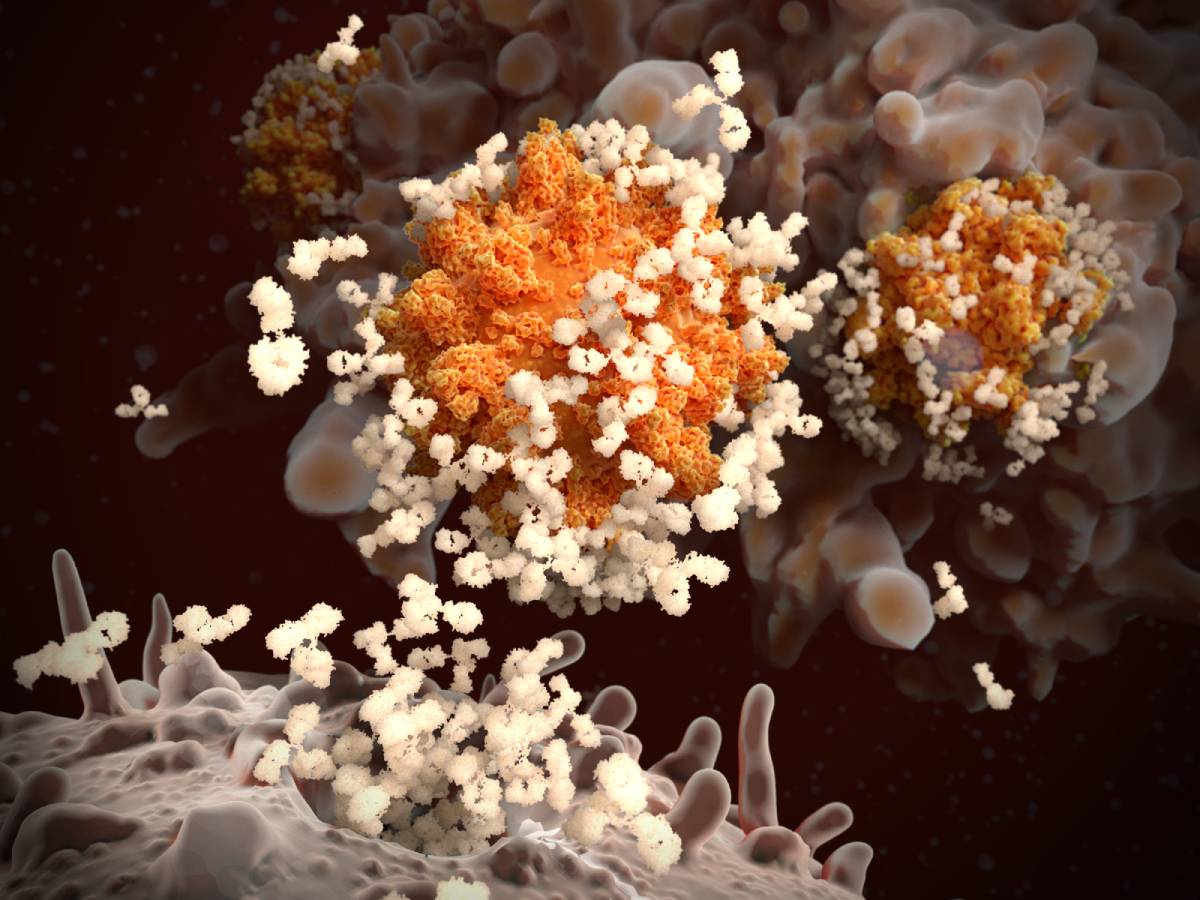
Immediately following SARS-CoV-2 infection, the replication and release of the virus kills the host cell, causing the production of proinflammatory signals such as cytokines and chemokines by neighboring cells (1). Leukocytes such as T cells rush to the site of infection, causing further inflammation, which either leads to organ damage in dysfunctional reactions or, alternatively, virus neutralization and recovery in healthy responses (1). To adequately fight the virus, the immune system must produce two types of T cells — CD4+ and CD8+ — that can quickly recognize SARS-CoV-2 and B cells that can produce neutralizing antibodies (1, 2). Because CD4+ T cells are essential for priming B cells, T cell production is crucial for an adequate response (2, 3). Detectable levels of T and B cell responses appear in the blood approximately 1 week after symptom onset (1). Roughly 2 weeks after the initial infection, individuals typically begin seroconversion, resulting in the presence of SARS-CoV-2-specific antibodies targeting the virus spike proteins by B cells (1, 3). Therefore, in simple terms, T cells are responsible for identifying the virus and triggering B cells, which are responsible for producing antibodies that can kill the virus (2).
After infection, the immune system retains T and B cell memory generated by the immune response (3). Studies have shown that convalescent COVID-19 patients produce CD8+ T cells with phenotypes similar to those produced by recently infected individuals, indicating that T cells keep the ability to identify the virus and promote immune responses long-term after the original infection (4). High levels of CD4+ T cells also circulate in the blood until at least six months post-infection (4). Additionally, one study found that 98% of convalescent individuals produced antibodies targeting the virus spike protein one month after infection, which remained stable until slowly declining 6 to 8 months later (5). In this study, the production of virus-specific B cells actually increased over time, peaking at 6 months post-infection (5). Other studies have found that long-lived bone marrow plasma cells specifically produce anti-spike protein immunoglobulin for at least 7 months following infection (6). However, the presence of these antibodies are not the only defense — some memory B cells can rapidly differentiate into virus-specific antibody producers after re-exposure to a pathogen (6). Thus, while the amount of SARS-CoV-2-specific antibodies and T cells may decline in the months following COVID-19 infection, the long-term memory of T and B cells usually allows the immune system to retain protective immunity and respond quickly to re-exposure long after the symptoms have disappeared, with relatively low chances of viral re-infection (3, 4).
While more research must be conducted, these findings have provided hope to public health efforts against COVID-19. Vaccinated patients also mount encouraging long-term responses to the virus (3), especially individuals who were both previously infected and vaccinated (7).
References
1: Tay, M., Poh, C., Renia, L., MacAry, P. and Ng, L. (2020). The trinity of COVID-19: immunity, inflammation, and intervention. Nature Reviews Immunology, vol. 20. DOI: 10.1038/s41577-020-0311-8.
2: Murchu, E., Byrne, P., Walsh, K., Carty, P., Connolly, M., Gascun, C., Jordan, K., Keoghan, M., O’Brien, K., O’Neill, M., Smith, S., Teljeur, C., Ryan, M., and Harrington, P. (2020). Immune response following infection with SARS-CoV-2 and other coronaviruses: a rapid review. Reviews in Medical Virology, vol. 31. DOI: 10.1002/rmv.2162.
3: Kim, D., Rowland-Jones, S. and Gea-Mallorqui, E. (2020). Will SARS-CoV-2 infection elicit long-lasting protective or sterilizing immunity? Implications for vaccine strategies. Frontiers in Immunology, vol. 11. DOI: 10.3389/fimmu.2020.571481.
4: Canate, P. and Vinuesa, C. (2020). COVID-19 makes B cells forget, but T cells remember. Cell, vol. 183. DOI: 10.1016/j.cell.2020.09.013.
5: Dan, J., Mateus, J., Kato, Y., Hastie, K., Yu, E., Faliti, C., Grifoni, A., Ramirez, S., Haupt, S., Frazier, A., Nakao, C., Rayaprolu, V., Rawlings, S., Peters, B., Krammer, F., Simon, V., Saphire, E., Smith, D., Weiskopf, D., Sette, A. and Crotty, S. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science, vol. 371. DOI: 10.1126/science.abf4063.
6: Turner, J., Kim, W., Kalaidina, E., Goss, C., Rauseo, A., Schmitz, A., Hansen, L., Haile, A., Klebert, M., Pusic, I., O’Halloran, J., Presti, R. and Ellebedy, A. (2021). SARS-CoV-2 infection induces long-lived bone marrow plasma cells in humans. Nature, vol. 595. DOI: 10.1038/s41586-021-03647-4.
7: Cho, A., Mueksch, F. and Nussenzweig, M. (2021). Anti-SARS-CoV-2 receptor binding domain antibody evolution after mRNA vaccination. Nature. DOI: 10.1038/s41586-021-04060-7.
