Erector Spinae Plane Block
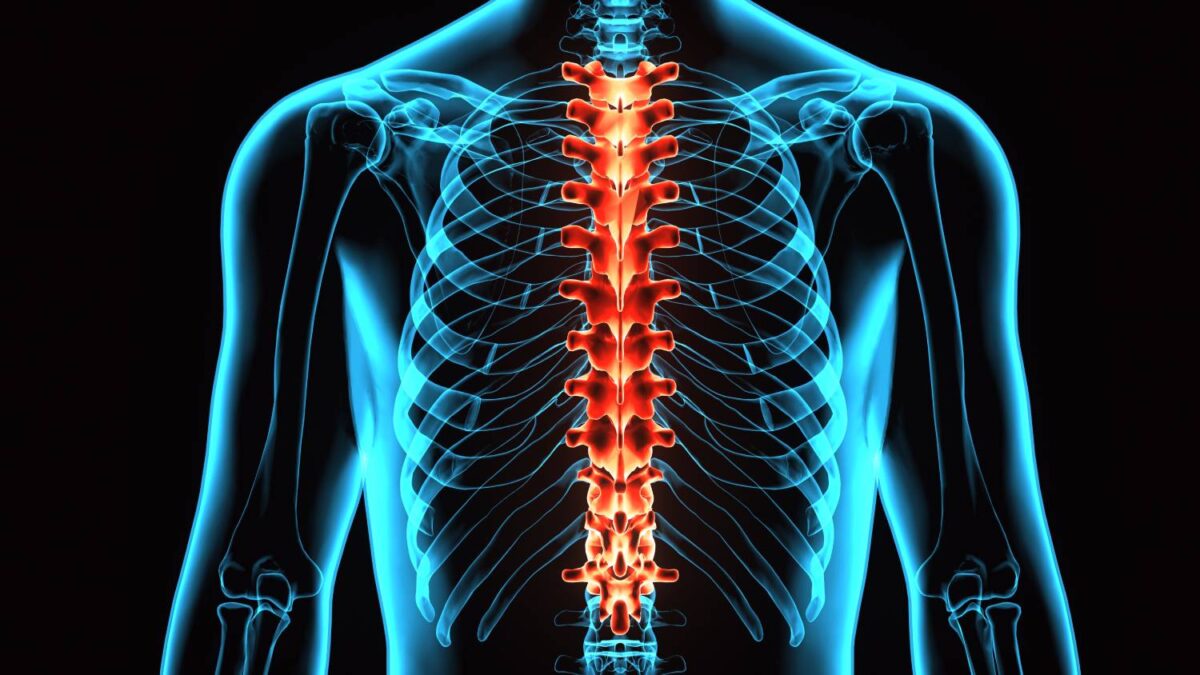
The erector spinae plane block (ESPB) is a novel form of neuropathic pain control and is also used for analgesia in certain surgical procedures [1]. When applied bilaterally at the T5 spinous process, ESPB can provide patients with analgesia from the T2 to T9 sensory level [2]. In practice, this means that ESPB can be used on patients in many different situations, including chronic shoulder pain treatment (T2), thoracic surgery (T4-5), mastectomy (T4-5), and upper abdominal surgery (T7-8) [3]. From infants to adults, patients of all ages have found their pain significantly alleviated due to ESPB [3]. Given the technique’s simplicity, safety, and versatility, ESPB is a prime candidate for postoperative pain control.
One benefit of ESPB is the ease with which it is administered. Other methods of managing neuropathic pain, such as pulsed radiofrequency and intrathecal injection of medications, run the risk of serious complications [1]. They are also very demanding: highly experienced personnel must administer them in invasive ways [1]. ESPB does not carry these risks. During ESPB administration, the needle must reach the transverse process, an easily identifiable landmark [4]. Furthermore, delicate structures, such as neuraxial anatomy and the pleura, are located far away from the needle, thereby reducing the risk of complication [4].
Not only is ESPB safer than other pain management techniques, but it can provide comparable if not better analgesia in certain contexts. Song et al. found that liposomal bupivacaine-based single-shot bilateral ESPB could reduce opioid consumption over the short-term for cardiac surgery patients [2]. Another study similarly documented how ESPB administered to lung transplant patients resulted in well-managed pain and improved oxygen saturation [5]. In this case, ESPB was compared to intercostal block [3]. Thoracotomy patients in the ESPB group reported lower static and dynamic pain scores and few complications [3].
However, ESPB is not always the most effective pain management option in all cases. For instance, one study compared the efficacy of ultrasound-guided intercostal nerve block (ICNB), multiple-injection paravertebral block (PVB), and ESPB during thoracoscopic surgery [4]. The experimenters identified PVB as the superior analgesic method [4]. While ESPB and ICNB reduced pain in comparable amounts, patients who received PVB reported significantly lower visual analog scale pain scores than any other group [4]. ESPB also decreased pain scores less than ultrasound-guided modified pectoral nerve block in a study focused on radical mastectomy patients [6].
Just as the type of surgery being performed may affect a physician’s decision to perform ESPB or not, a patient’s history with opioid reliance must also factor into this decision. Some studies, such as Mudarth et al.’s examination of lung transplant patients, report that ESPB leads to decreased narcotic consumption, compared to other alternatives [5]. Meanwhile, other experiments focused on mastectomy and cardiac patients have noted no significant long-term difference in patients’ opioid consumption [2, 6]. This lack of consensus may be due to a lack of large studies rather than a significant difference across types of surgeries. Further research is necessary to inform how physicians should factor patients’ history of opioid use into the decision to administer ESPB.
Ultimately, ESPB is a promising analgesic method that could significantly help manage and reduce incidences of neuropathic pain, as well as manage postoperative pain for surgeries in the torso area. It is a safe and versatile method of pain control, but its comparative success in managing pain and reducing opioid consumption requires further investigation.
References
[1] M. Forero et al., “The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain,” Regional Anesthesia & Pain Medicine, vol. 41, no. 5, p. 621-627, September-October 2016. [Online]. Available: https://doi.org/10.1097/AAP.0000000000000451.
[2] K. Song et al., “Liposomal Bupivacaine-Based Erector Spinae Block for Cardiac Surgery,” Journal of Cardiothoracic and Vascular Anesthesia, vol. 35, no. 5, p. 1555-1559, May 2021. [Online]. Available: https://doi.org/10.1053/j.jvca.2020.09.115.
[3] F. D. Geyik et al., “Evaluation of Analgesic Effectiveness of Continuous Erector Spinae Plane Block in Patients Undergoing Thoracotomy,” Journal of the Society of Thoracic Cardiovascular Anaesthesia & Intensive Care, vol. 26, no. 4, p. 189-196, October 2020. [Online]. Available: https://doi.org/10.5222/GKDAD.2020.93899.
[4] N. Chen et al., “The effect of ultrasound-guided intercostal nerve block, single-injection erector spinae plane block and multiple-injection paravertebral block on postoperative analgesia in thoracoscopic surgery: A randomized, double-blinded, clinical trial,” Journal of Clinical Anesthesia, vol. 59, p. 106-111, February 2020. [Online]. Available: https://doi.org/10.1016/j.jclinane.2019.07.002.
[5] M. Mudarth et al., “Continuous Erector Spinae Plane Block for Analgesia after Thoracotomy for Lung Transplantation in an Anticoagulated Patient,” Case Reports in Anesthesiology, vol. 2021, p. 1-4, February 2021. [Online]. Available: https://doi.org/10.1155/2021/6664712.
[6] B. Altıparmak et al., “Liposomal Bupivacaine-Based Erector Spinae Block for Cardiac Surgery,” Journal of Clinical Anesthesia, vol. 54, p. 61-65, May 2019. [Online]. Available: https://doi.org/10.1016/j.jclinane.2018.10.040.
