Use of the Sitting Position in Anesthesia
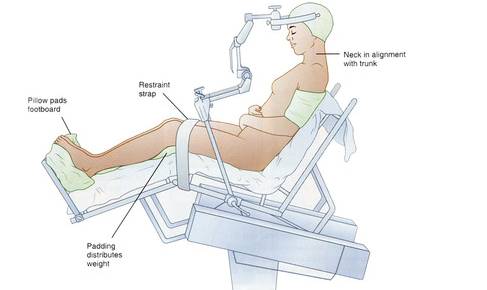
Anesthesia for surgery performed in the sitting position presents unique challenges and considerations for anesthesiologists due to the physiological and mechanical implications of patient positioning. Historically preferred for certain posterior fossa, cervical spine, and shoulder surgeries, this technique offers improved surgical exposure, reduced bleeding, and, for neurosurgery, better cerebrospinal fluid drainage. However, it is associated with significant risks, including venous air embolism (VAE), hemodynamic instability, and challenges in airway management (1).
One of the primary concerns associated with anesthesia and surgery in the sitting position is the increased risk of VAE. This occurs when negative venous pressure allows air to enter the central venous system, which can lead to pulmonary obstruction, right ventricular dysfunction, and even paradoxical embolism if there is a right-to-left shunt (1). A large retrospective analysis of 1,000 cases found that the detection and management of VAE has improved with advancements in monitoring techniques, including precordial Doppler ultrasound and transesophageal echocardiography (TEE). The study emphasized that early recognition and prompt intervention, including repositioning, hemodynamic support, and aspiration of entrained air through a central venous catheter, are critical to reducing the risk of serious complications (1).
Another major challenge in anesthesia management for surgery in the sitting position is maintaining hemodynamic stability. The gravitational effects of this position result in decreased venous return, decreased cardiac output, and potential hypotension (2). Pediatric patients undergoing neurosurgery in the sitting position were found to be particularly susceptible to hemodynamic fluctuations compared to those in the park-bench position. A study by Radu et al. found that aggressive fluid resuscitation, continuous vasopressor infusion, and careful monitoring of intravascular volume status could help maintain stable perfusion pressures (2). In addition, controlled ventilation strategies and avoidance of excessive positive end-expiratory pressure (PEEP) may prevent adverse cerebrovascular effects.
Management of anesthesia in the sitting position also requires careful airway control. Endotracheal intubation is standard, but the head’s flexed position can make airway access difficult if reintubation is required intraoperatively (3). A case report detailing perioperative management of a super-obese patient undergoing endoscopic neurosurgery highlighted the increased complexity of airway control due to excessive adipose tissue and limited neck mobility. The authors recommended advanced airway devices, fiberoptic intubation, and close collaboration between the anesthesia and surgical teams to optimize airway safety (3).
Another rare but notable complication associated with surgery in the sitting position is the Bezold-Jarisch reflex (BJR), which is characterized by profound bradycardia, hypotension, and vasodilation. This reflex is thought to be triggered by venous pooling and decreased cardiac filling pressures, resulting in excessive vagal activation (4). A case study reported the occurrence of BJR after endoscopic endonasal resection of a clival tumor. The patient experienced severe hypotension and bradycardia requiring immediate administration of atropine and fluid resuscitation. The authors emphasized the importance of vigilant monitoring, early intervention with vasopressors, and volume expansion to prevent and manage this reflex (4).
Despite these risks, the sitting position continues to be used in select surgical cases due to the visualization that it allows. Advancements in intraoperative monitoring, anesthetic techniques, and surgical strategies have significantly improved patient safety. Careful patient selection, preoperative screening for risk factors such as patent foramen ovale (which predisposes to paradoxical embolism), and individualized anesthetic plans are critical to optimizing outcomes. Through careful perioperative management, vigilant hemodynamic monitoring, and rapid response to complications, anesthesiologists play a critical role in balancing the benefits of the sitting position with its associated risks.
References
- Hurth H, Ebner FH, Clement E, et al. The risk of intraoperative venous air embolism from neurosurgical procedures performed in the lounging position: an in-depth analysis of detection, management, and outcomes of 1000 consecutive cases. J Neurosurg. 2024;142(3):797-807. Published 2024 Sep 20. doi:10.3171/2024.5.JNS232449
- Radu OM, Balaci GM, Leucuţa DC, Florian IŞ. Exploring anesthesia-related complications in pediatric neurosurgery: a comparative analysis of the sitting and park-bench positions. Med Pharm Rep. 2024;97(4):540-548. doi:10.15386/mpr-2788
- Ogiwara T, Sato A, Nakamura K, et al. Perioperative management of craniopharyngioma resection through endoscopic endonasal approach in a super-super obese patient: A technical case report. Surg Neurol Int. 2025;16:11. Published 2025 Jan 10. doi:10.25259/SNI_856_2024
- Peterson A, Hussain O, Zwagerman N, Woehlck H. The Bezold-Jarisch Reflex Following an Endoscopic Endonasal Resection of an Intraosseous Clival Myxoma: A Case Report. Case Rep Anesthesiol. 2025;2025:3336045. Published 2025 Feb 20. doi:10.1155/cria/3336045
